By Krysty Radabaugh, BS, MS, R.T., (R)(CT)(MR)
Director of Operations, and Chief MRI Technologist
All-American Teleradiology
MRI is the imaging modality of choice for evaluation of musculoskeletal pathology of the ankle and foot, including soft tissue, osseous trauma, neoplasms, and inflammatory pathology. MRI provides superior resolution and exquisite detail of soft tissue structures using multiplanar capabilities. However, MRI of the foot and ankle can be challenging for time consuming for radiologists as the foot contains 28 bones and 30 joints. Proper positioning, protocol consultation with an experienced Musculoskeletal Radiologist, and consultation with the referring physician can improve the performance of MRI as a diagnostic tool. All-American Teleradiology provides MRI technologist consultation, MRI accreditation assistance and a team of Musculoskeletal Radiologists readily available for accurate interpretations.
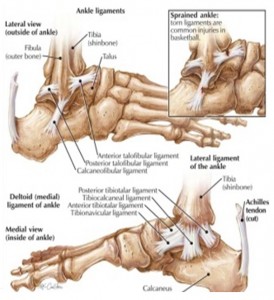
Soft-tissue disorders examples include: Ligaments (sprain/tear) and Tendons (Tendinosis, Peritendinitis, Tenosynovitis, Entrapment, Tear, Rupture, Dislocation),
Syndrome examples include: Anterolateral Impingement syndrome, Sinus Tarsi syndrome, Compressive neuropathies (Tarsal tunnel syndrome, Morton neuroma), and synovial disorders.
MRI imaging has also been shown to be highly sensitive in the detection and staging of a number of infections including: Cellulitis, Soft-Tissue abscesses, and Osteomyelitis.
MRI imaging is excellent for the early detection and assessment of a number of osseous abnormalities such as bone contusions, stress and insufficiency fractures, osteochondral fractures, osteonecrosis, and transient bone marrow edema. It is increasingly being recognized as the modality of choice for assessment of pathologic conditions of the ankle and foot. It far surpasses CT in the evaluation of trabecular bone injury.
TECHNOLOGIST ROLE:
 The Technologist role is crucial in helping to identifying injury or infection. Positioning of the ankle and foot correctly is the second step to an accurate diagnosis, along with correct imaging sequences, markers and the use of contrast materials. The critical first step is the history of the injury and area to be imaged. Some physicians assume when a foot/ankle is ordered they will receive an interpretation for the foot that includes ankle pathology. For example, the posterior tibial tendon should be imaged as an ankle not a foot. Or a Podiatrist requests Plantar Fascia vs. Plantar Fasciitis. It can be scanned as a hindfoot/ankle however many Podiatrist want to see the attachment into the forefoot. If midfoot or forefoot is desired, these will generally need to be ordered and scheduled as separate studies.
The Technologist role is crucial in helping to identifying injury or infection. Positioning of the ankle and foot correctly is the second step to an accurate diagnosis, along with correct imaging sequences, markers and the use of contrast materials. The critical first step is the history of the injury and area to be imaged. Some physicians assume when a foot/ankle is ordered they will receive an interpretation for the foot that includes ankle pathology. For example, the posterior tibial tendon should be imaged as an ankle not a foot. Or a Podiatrist requests Plantar Fascia vs. Plantar Fasciitis. It can be scanned as a hindfoot/ankle however many Podiatrist want to see the attachment into the forefoot. If midfoot or forefoot is desired, these will generally need to be ordered and scheduled as separate studies.
As a general rule, the entire foot should never be scanned as a single study. This precludes optimizing scan planes, pulse sequences, and positioning for specific structures, and spatial resolution will be inadequate. Some referring physicians are not aware of this and the technologist must therefore be proactive in clarifying the region of interest as forefoot, midfoot, or hindfoot/ankle, in consultation with the radiologist if necessary.
MRI INDICATIONS FOOT:
The foot and ankle are the hardest area to image due to area ordered, positioning and imaging plane for hindfoot(ankle), midfoot and forefoot.
Hindfoot/Ankle:
 Plantar fasciitis is best seen within 2 to 3 cm of the calcaneal attachment. Edema may be seen in the calcaneus at the insertion site of the plantar fascia. Planter calcaneal spurs are common in approximately 50% of cases. A tear of the plantar fascia most commonly occur in the midportion of the fascia being partial or complete and are common from a traumatic injury.
Plantar fasciitis is best seen within 2 to 3 cm of the calcaneal attachment. Edema may be seen in the calcaneus at the insertion site of the plantar fascia. Planter calcaneal spurs are common in approximately 50% of cases. A tear of the plantar fascia most commonly occur in the midportion of the fascia being partial or complete and are common from a traumatic injury.
Plantar fibromatosis is nodular fibrous proliferation of the plantar fascia and can be ordered as: pain in foot/soft tissue mass. Contrast use should be checked with Radiologist.
Diagnosis of other abnormalities including fracture, calcaneal pain, os trigonum syndrome, subtalar coalition, talar dome OCD and Achilles insertion issues.
Midfoot:
Depending on the patient population, common diagnoses include metatarsal stress fractures or neuropathic arthropathy often with a question of osteomyelitis. A traumatic tear of the Lisfranc ligament can lead to instability and progressive disorganization of the Lisfranc joint. Additionally, there can be loss of the medial longitudinal arch. The rupture of the ligament fibers is more common than is the avulsion fracture at the bony attachments.
The tarsal bones are a common site of trabecular stress injury. Marrow edema with a lack of a clear fracture line is present.
The flexor hallucis longus (FHL) occasionally becomes entrapped in the midfoot due to lesions about the Knot of Henry (“jogger’s foot”). The mechanism is chronic repetitive friction with the flexor digitorum longus (FDL) tendon.
Forefoot:
“Turf Toe” refers to a capsuloligamentous injury of the metatarsophalangeal (MTP) joint of the first toe. The mechanism of injury includes anterior thrust of the metatarsal head in a hyperextended joint with a relatively fixed great toe. This is common in sports played on synthetic turf . . . football, soccer and baseball. There is stretching and tearing of the plantar capsule and tearing of the plantar plate. The plantar plate is a fibrocartilaginous structure that extends from the metatarsal neck to the base of the proximal phalanx. It reinforces the plantar capsule and also attaches the hallux sesamoid bones to the base of the proximal phalanx.
Other common forefoot pathologies in which MRI can be critical include skimboarder’s toe (tear of dorsal capsul), symptomatic hallux valgus (bunion), seasmoid fx/avn, morton’s neuroma, lesser mtp plantar plate tear, and the occasional OCD.
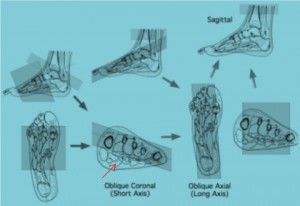
Foot Imaging Planes:
Angle parallel to the 2nd and 3r metatarsal heads on your oblique Coronal
ANKLE/HINDFOOT POSITIONING AND ANATOMY:
The most frequently diseased tendons in the ankle are the Achilles, posterior tibial, and peroneal. MRI can be used to diagnose most disorders of these tendons, as well as stage these disorders to allow appropriate therapy.
Achilles imaging must cover to gastrocnemius insertion
Designated imaging planes Ankle for PTT and Peroneal Pathology
CONCLUSION:
MRI is the gold standard for foot/ankle traumatic injuries and diagnosis of chronic pain/instability syndromes. The high cost of healthcare often puts the patient in the difficult position of determining if a diagnostic test makes economic sense. To help ensure that the referring physician and their patients get true value from the MRI, consult with the ordering Physician and Musculoskeletal Radiologist prior to exam. The right imaging techniques, outstanding image quality and a clinically specific report will ensure optimal diagnosis and treatment for patients.
All-American Teleradiology provides rapid, accurate decisive musculoskeletal MRI interpretations performed by highly experienced, fellowship trained Musculoskeletal Radiologists. Our value added consultative MRI services, to include our providing free MRI accreditation assistance and a Medical Director can help ensure appropriate reimbursement and the highest level of clinical performance.
For more information, email Krysty@allamericanrad.com, call 888-365-5514 or visit www.allamericanrad.com.
Krysty Radabaugh has over 20 years of MRI experience in hospital and outpatient settings. She has served as MRI Coordinator for Cleveland Clinic hospitals; Technical Director for Franklin & Seidelmann Teleradiology; and MRI Accreditation Specialist with national MRI center chain. She has managed MRI centers utilizing a wide range of MRI equipment, which includes: Hitachi, Phillips, GE, Siemens, Toshiba and Esaote. Ms. Radabaugh has worked as a MRI Applications Specialist with Hitachi and Consultant to GE Medical and Bayer Healthcare.