Overhaul the Antiquated Out-of-State Medical Licensure Bureaucracy
 By Shella Farooki, M.D.
By Shella Farooki, M.D.
Radiologist
All-American Teleradiology
August 31, 2020
While national politicians and other governors are mired in partisan disputes, Governor Mike DeWine is rising above the fray to find evidence-based solutions to the COVID-19 pandemic. As an Ohio doctor who works in our state and others, I applaud DeWine’s focus on saving lives. And I urge him to go further by renewing, expanding, and making permanent Executive Order 2020-01D before it expires in September to allow out-of-state physicians to practice without an Ohio license.
In May, DeWine signed Executive Order 2020-01D to allow nurses the emergency permission to start practicing medicine as soon as they get their licenses. The Executive Order also sped up the licensing process for out-of-state nurses for the duration of the pandemic. These measures helped get more medical personnel on the ground as COVID-19 spread. They strengthened Ohio’s medical facilities. And they proved that rescinding unnecessary licensing restrictions for another qualified class of medical professional – physicians – will improve Ohioans’ health and welfare.
The difference between current out-of-state physician licensing standards and those for nurses are night and day. As of this writing, licensed and qualified out-of-state physicians must go through a time-consuming and expensive process to become licensed. This government interference in the patient-physician relationship increases costs and decreases care in both normal times and emergencies. Meanwhile, nurses can get to work practically the same day on which they receive their license.
The reality is that complex licensing regimes aren’t practical even when there is no public health emergency. Making a fully-trained and qualified medical professional take yet another test won’t improve patient care, and refusing to recognize a qualification they earned in another state worsens patient care. Permanently expanding the emergency declarations for nurses to physicians would improve patient health, decrease patient costs, and create statewide consistency for medical professionals. And it would remove another layer of bureaucracy which separates us from our patients.
This isn’t a theoretical problem. I’ve been a physician for 20 years, half of that engaged in teleradiology, and I’m licensed to practice in 15 states. Despite my qualifications, I’ve been waiting for three months to get relicensed in Georgia because the state’s licensing bureaucracy keeps crossing threads with licensing bureaucracies in other states. If the COVID-19 hotspots spread, and Georgia needed physicians on short notice, I can’t help – even though telemedicine makes me available to any patient in any part of Georgia at virtually any time.
The same is true for an out-of-state physician coming to Ohio to help fight the pandemic.
From emergency occupational licensing rescissions to the announcement last week of an interstate testing pact, DeWine has proven that partisan politics takes a back seat to Ohioan’s safety. But emergencies don’t just happen when someone contracts a pandemic virus; for the average family, an emergency like a car accident or a heart attack could happen any day. Unfortunately, it’s been difficult for many Ohioans to see their primary care physician, let alone a specialist, throughout the past few months. We have to do everything we can to prevent an even more serious shortage of physicians in the future – the kind that turns a routine healthcare need into a crisis. Making it easier for physicians from other states to practice here would help us quickly scale responses to future emergencies, expand healthcare access, and reduce costs for families.
As the coronavirus continues to divide Americans on partisan lines, I urge Governor DeWine to act in the best interests of patients by renewing, expanding, and making permanent EO 2020-01D. It will help Ohio now and forevermore empower the best care through the best method: a strong patient-physician relationship.
Dr. Shella Farooki is a Board-Certified, Fellowship-Trained radiologist specializing in musculoskeletal imaging. She resides in Dublin, Ohio, and provides interpretative consultations to physician practices throughout the United States via All-American Teleradiology.
Finger Pulleys – Patterns of Pathology
 By Peter Louis Glickman, M.D.
By Peter Louis Glickman, M.D.
All-American Teleradiology
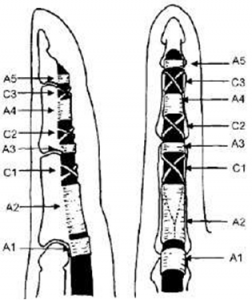
Finger pulleys are fine annular and cruciform structures, which hold the flexor tendons close to the phalanges and joints of the fingers and thereby facilitate strong and complete flexion of the digits in response to muscular contraction distant from the sites of mechanical action. Their anatomic arrangement in the second through fifth fingers is shown in Fig 1.
(Hauger 2000)
Fig 1. 2nd-5th finger pulley anatomy
Pulley anatomy of the thumb is somewhat different (Fig 2).
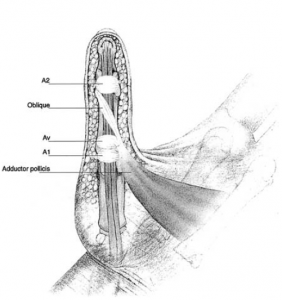
(Bayat 2002)
Fig 2. Thumb pulley anatomy
Some common anatomic variations of have been described as well (Bayat 2002).
Annular pulleys are classically subject to 4 main pathologies (Moutet 2003, Makkouk 2007):
- Trigger finger – chondroid metaplasia, usually of the A1 pulley, associated with stenosing tenosynovitis. Usually idiopathic, occurring in women in the 5th and 6th decades of life (F:M 6:1), most commonly thought to be due to a genetic predisposition. May also occur in rheumatoid arthritis, gout, diabetes mellitus (associated with duration of disease, not glycemic control), renal disease, amyloidosis, hypothyroidism, and connective tissue disorders. Ring finger most commonly affected, followed by thumb, long, index, and small fingers. Can be multiple.
- Tenosynovial ganglions – arise more commonly at a weak point between the A1 and A2 pulleys.
- Traumatic/surgical injuries to the tendon sheath.
- Overuse or stress ruptures of the annular pulleys, e.g. classically with rock climbing, but more recently shown in baseball pitchers too (Lourie 2010). Rock climbers typically injure distal aspect of the A2 pulley, with involvement of A3 and A4 in more severe injuries, related to crimping posture (DIP hyperextension and PIP hyperflexion). Baseball pitchers were shown in a small series to suffer isolated middle finger A4 injuries, thought to be related to repetitive ball-induced extension moments on an acutely flexed DIP joint when throwing fastballs (Lourie 2011). A2 pulley injuries have also been described in bowlers (Patel 2012).
#1 and #4 will be covered in this article.
Normal Anatomy
Annular and pulleys are arranged as in Fig 1, and are thin markedly hypointense structures on MR imaging connecting the flexor tendons to the phalanges and joints, best directly visualized on axial images. Cruciform pulleys are only rarely visualized on imaging due to their extremely small size.
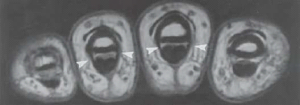
Fig 3. Arrowheads depict annular pulleys in cross section
On sagittal images, the next most useful images to evaluate for pulley injuries, the flexor tendons should be 1mm or less away from their adjacent phalanges.
Finger Pulley Injuries
With the rise in popularity of the sport of rock climbing in the 1980’s, closed finger pulley ruptures began to appear. Competitive climbers routinely put their entire body weight (and more during maneuvers) on one or two flexed fingers. Pulley lesions have been shown to be the single most common injury in these athletes (Schoff 2003).
Pulley lesions are most commonly seen in the ring and middle fingers and may be diagnosed in up to 30% of finger injuries. Fixed contracture of the PIP joint may result if timely diagnosis and treatment is not rendered.
Imaging is performed to clarify the severity and extent of pulley injury, as well as to exclude mimics such as tenosynovitis, tendon tear, or adjacent osseous or soft tissue injury. In young sport climbers, imaging is advisable to exclude epiphyseal fracture and epiphysiolysis (Hochnolzer 2005), preferably with both radiographs and MR as complementary modalities. CT should be reserved for problem-solving in cases of questionable fractures.
On sagittal MR and US images, more than 1mm of separation between the flexor tendons and phalanges is abnormal and is termed “bowstringing”, the extent of which generally reflects the severity and extent of the injuries, e.g. 2-5 mm in isolated complete single pulley ruptures, and 5-8 mm in simultaneous complete tears of multiple pulleys. Partial tears of annular pulleys result in bowstringing as well, typically to a lesser extent. Forced flexion is an important maneuver to elicit increase bowstringing in subtle cases. This may be much easier to image on focused ultrasound examination compared to MRI, due to the ease of provocation and much shorter required duration of flexion (which is often painful for injured patients).
Pulleys are seen to be either frankly torn in the case of a rupture, or thickened, thinned, and/or indistinct in the case of partial tears. Bowstringing is appreciable on sagittal as well as axial images.
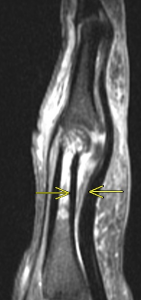
Fig 4a. Complete rupture of the A2 pulley (a – sagittal T2 fat-saturated MRI, b – axial T2 fat-saturated MRI ). Arrows depict bowstringing related to complete rupture of the A2 pulley
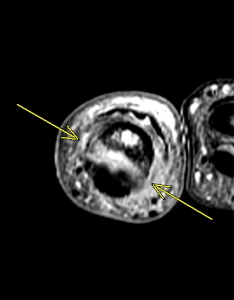
Fig 4b. Complete rupture of the A2 pulley (a – sagittal T2 fat-saturated MRI, b – axial T2 fat-saturated MRI ). Arrows depict bowstringing related to complete rupture of the A2 pulley

Fig 5a. Partial tear of A2 pulley. Arrows depict mild bowstringing related to partial tear of A2 (Clavero 2002) (a – sagittal MRI, b – axial MRI).
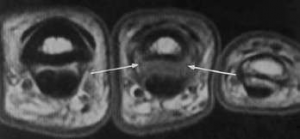
Fig 5b. Partial tear of A2 pulley. Arrows depict mild bowstringing related to partial tear of A2 (Clavero 2002) (a – sagittal MRI, b – axial MRI). Arrows depict attenuation and indistinctness of the medial and lateral aspects of the A2 pulley in T1 weighted images, consistent with partial tear.
Schoff (2006) classified pulley inuries in rock climbers as follows:
Grade I – Pulley strain
Grade II – Complete rupture of A4 or partial rupture of A2 or A3
Grade III – Complete rupture of A2 or A3
Grade IV – Multiple ruptures as A2/A3, A2/A3/A4, or single rupture (A2 or A3) combined with lumbricalis muscles or collateral ligament trauma. Current concepts favor surgery only in the case of a Type IV injury.
Trigger Finger
The A1 pulley is subjected to the highest stresses of all the pulleys, during normal and power-grip due to its location. Repeated threading of the flexor tendons through the A1 pulley can cause friction and result in intratendinous swelling, similar to fraying of a string with repeated threading through the eye of a needle. Electron microscopy has revealed fibrocartilagenous metaplasia and Type III collagen proliferation coating the pulley’s innermost layer as the precipitating pathologic lesion (Makkouk 2007).
Usually diagnosed clinically, trigger finger is imaged to localize the anatomic lesion and evaluate for rare mimics and associated pathologies, such as partial tendon tears or adhesions, or nodular tendinosis. MRI and US both demonstrate findings of thickening and inflammation of the A1 pulley, and post-gadolinium contrast images may demonstrate pulley enhancement, as in Fig 6..
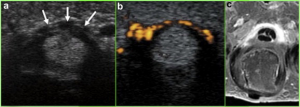
Fig. 6. Arrows depict A1 pulley hypertrophy on US, with Power Doppler demonstrating hyperemia, and post-contrast T1 fat-suppressed MRI demonstrating pulley enhancement (Vuillemin 2012)
Nodular tendinosis may be associated (Fig 7).
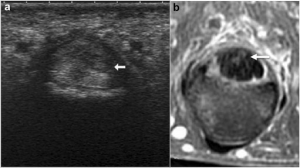
Fig 7. Arrows depict hypoechoic nodule on US, hyperintense on T2-weighted MRI (Vuillemin 2012)
Tenosynovial fluid and membrane thickening may also be seen, as with other stenosing tenosynovial processes such as De Quervain’s syndrome.
Traditionally treated with splinting, clinically guided corticosteroid injection, or surgical release, success with ultrasound-guided corticosteroid injection has also recently been reported, with 90% success rate in at 12 months, and 71% at year 3 (Bodor 2009).
Conclusion
Patterns of traumatic and non-traumatic pathologies of the finger pulleys are diverse, and important to recognize and accurately classify on imaging. Understanding these patterns is crucial to accurate and timely diagnosis to avoid complications, and to minimize time away from competitive or recreational activities.
All-American Teleradiology provides rapid, accurate decisive musculoskeletal MRI interpretations performed by highly experienced, fellowship trained Musculoskeletal Radiologists. Our value added consultative MRI services, to include our providing free MRI accreditation assistance and a Medical Director can help ensure appropriate reimbursement and the highest level of clinical performance.
For more information, email info@allamericanrad.com, call 888-365-5514 or visit www.allamericanrad.com.
Peter Louis Glickman, M.D.
Musculoskeletal Specialist, Foot & Ankle
All-American Teleradiology
Mark E. Pruzansky, M.D.
Assistant Clinical Professor of Orthopaedic Surgery
Icahn School of Medicine at Mount Sinai, New York, N.Y.
References
- Bayat A, Shaaban H, Giakas G, Lees VC. J Hand Surg Am. 2002 Jul;27(4):628-35. The pulley system of the thumb: anatomic and biomechanical study.
- Bodor M, Flossman T. J Ultrasound Med. 2009 Jun;28(6):737-43. Ultrasound-guided first annular pulley injection for trigger finger.
- Clavero JA, Alomar X, Monill JM, Esplugas M, Golanó P, Mendoza M, and Salvador A. Radiographics March 2002 22:2 237-256. EDUCATION EXHIBIT – Continuing Medical Education: MR Imaging of Ligament and Tendon Injuries of the Fingers.
- El-Sheikh Y, Wong I, Farrokhyar F, and Thoma A. Can J Plast Surg. 2006 Winter; 14(4): 227–231. PMCID: PMC2686056 Diagnosis of finger flexor pulley injury in rock climbers: A systematic review.
- Hauger O, Chung CB, Lektrakul N, Botte MJ, Trudell D, Boutin RD, Resnick D. Radiology. 2000 Oct;217(1):201-12. Pulley system in the fingers: normal anatomy and simulated lesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath.
- Hochholzer T, Schöffl VR. Wilderness Environ Med. 2005 Fall;16(3):139-42. Epiphyseal fractures of the finger middle joints in young sport climbers.
- Klauser A, Frauscher F, Bodner G, Halpern EJ, Schocke MF, Springer P, Gabl M, Judmaier W, zur Nedden D. Radiology. 2002 Mar;222(3):755-61. Finger pulley injuries in extreme rock climbers: depiction with dynamic US.
- Lourie GM, Hamby Z, Raasch WG, Chandler JB, Porter JL. Am J Sports Med. 2011 Feb;39(2):421-4. doi: 10.1177/0363546510387506. Epub 2010 Dec 20. Annular flexor pulley injuries in professional baseball pitchers: a case series.
- Makkouk AH, Oetgen ME, Swigart CR, and Dodds SD. Curr Rev Musculoskelet Med. 2008 June; 1(2): 92–96. Published online 2007 November 27. doi: 10.1007/s12178-007-9012-1 PMCID: PMC2684207 Trigger finger: etiology, evaluation, and treatment.
- Moutet F. Chir Main. 2003 Feb;22(1):1-12. [Flexor tendon pulley system: anatomy, pathology, treatment]. [Article in French]
- Patel P, Schucany WG, Toye L, and Ortinau E. Proc (Bayl Univ Med Cent). 2012 July; 25(3): 282–284. Flexor tendon pulley injury in a bowler.
- Schöffl VR, Schöffl I. J Hand Surg Am. 2006 Apr;31(4):647-54. Injuries to the finger flexor pulley system in rock climbers: current concepts.
- Vuillemin V, Guerini H, Bard H, Morvan G. J Ultrasound. 2012 Feb;15(1):20-8. doi: 10.1016/j.jus.2012.02.002. Epub 2012 Mar 9. Stenosing tenosynovitis.
The MRI Technologist Role in Foot/Ankle Positioning

By Krysty Radabaugh, BS, MS, R.T., (R)(CT)(MR)
Director of Operations, and Chief MRI Technologist
All-American Teleradiology
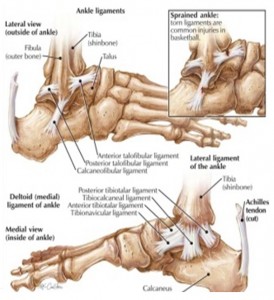
MRI is the imaging modality of choice for evaluation of musculoskeletal pathology of the ankle and foot, including soft tissue, osseous trauma, neoplasms, and inflammatory pathology. MRI provides superior resolution and exquisite detail of soft tissue structures using multiplanar capabilities. However, MRI of the foot and ankle can be challenging for time consuming for radiologists as the foot contains 28 bones and 30 joints. Proper positioning, protocol consultation with an experienced Musculoskeletal Radiologist, and consultation with the referring physician can improve the performance of MRI as a diagnostic tool. All-American Teleradiology provides MRI technologist consultation, MRI accreditation assistance and a team of Musculoskeletal Radiologists readily available for accurate interpretations.
Soft-tissue disorders examples include: Ligaments (sprain/tear) and Tendons (Tendinosis, Peritendinitis, Tenosynovitis, Entrapment, Tear, Rupture, Dislocation),
Syndrome examples include: Anterolateral Impingement syndrome, Sinus Tarsi syndrome, Compressive neuropathies (Tarsal tunnel syndrome, Morton neuroma), and synovial disorders.
MRI imaging has also been shown to be highly sensitive in the detection and staging of a number of infections including: Cellulitis, Soft-Tissue abscesses, and Osteomyelitis.
MRI imaging is excellent for the early detection and assessment of a number of osseous abnormalities such as bone contusions, stress and insufficiency fractures, osteochondral fractures, osteonecrosis, and transient bone marrow edema. It is increasingly being recognized as the modality of choice for assessment of pathologic conditions of the ankle and foot. It far surpasses CT in the evaluation of trabecular bone injury.
TECHNOLOGIST ROLE:
 The Technologist role is crucial in helping to identifying injury or infection. Positioning of the ankle and foot correctly is the second step to an accurate diagnosis, along with correct imaging sequences, markers and the use of contrast materials. The critical first step is the history of the injury and area to be imaged. Some physicians assume when a foot/ankle is ordered they will receive an interpretation for the foot that includes ankle pathology. For example, the posterior tibial tendon should be imaged as an ankle not a foot. Or a Podiatrist requests Plantar Fascia vs. Plantar Fasciitis. It can be scanned as a hindfoot/ankle however many Podiatrist want to see the attachment into the forefoot. If midfoot or forefoot is desired, these will generally need to be ordered and scheduled as separate studies.
The Technologist role is crucial in helping to identifying injury or infection. Positioning of the ankle and foot correctly is the second step to an accurate diagnosis, along with correct imaging sequences, markers and the use of contrast materials. The critical first step is the history of the injury and area to be imaged. Some physicians assume when a foot/ankle is ordered they will receive an interpretation for the foot that includes ankle pathology. For example, the posterior tibial tendon should be imaged as an ankle not a foot. Or a Podiatrist requests Plantar Fascia vs. Plantar Fasciitis. It can be scanned as a hindfoot/ankle however many Podiatrist want to see the attachment into the forefoot. If midfoot or forefoot is desired, these will generally need to be ordered and scheduled as separate studies.
As a general rule, the entire foot should never be scanned as a single study. This precludes optimizing scan planes, pulse sequences, and positioning for specific structures, and spatial resolution will be inadequate. Some referring physicians are not aware of this and the technologist must therefore be proactive in clarifying the region of interest as forefoot, midfoot, or hindfoot/ankle, in consultation with the radiologist if necessary.
MRI INDICATIONS FOOT:
The foot and ankle are the hardest area to image due to area ordered, positioning and imaging plane for hindfoot(ankle), midfoot and forefoot.
Hindfoot/Ankle:
 Plantar fasciitis is best seen within 2 to 3 cm of the calcaneal attachment. Edema may be seen in the calcaneus at the insertion site of the plantar fascia. Planter calcaneal spurs are common in approximately 50% of cases. A tear of the plantar fascia most commonly occur in the midportion of the fascia being partial or complete and are common from a traumatic injury.
Plantar fasciitis is best seen within 2 to 3 cm of the calcaneal attachment. Edema may be seen in the calcaneus at the insertion site of the plantar fascia. Planter calcaneal spurs are common in approximately 50% of cases. A tear of the plantar fascia most commonly occur in the midportion of the fascia being partial or complete and are common from a traumatic injury.
Plantar fibromatosis is nodular fibrous proliferation of the plantar fascia and can be ordered as: pain in foot/soft tissue mass. Contrast use should be checked with Radiologist.
Diagnosis of other abnormalities including fracture, calcaneal pain, os trigonum syndrome, subtalar coalition, talar dome OCD and Achilles insertion issues.
Midfoot:
Depending on the patient population, common diagnoses include metatarsal stress fractures or neuropathic arthropathy often with a question of osteomyelitis. A traumatic tear of the Lisfranc ligament can lead to instability and progressive disorganization of the Lisfranc joint. Additionally, there can be loss of the medial longitudinal arch. The rupture of the ligament fibers is more common than is the avulsion fracture at the bony attachments.
The tarsal bones are a common site of trabecular stress injury. Marrow edema with a lack of a clear fracture line is present.
The flexor hallucis longus (FHL) occasionally becomes entrapped in the midfoot due to lesions about the Knot of Henry (“jogger’s foot”). The mechanism is chronic repetitive friction with the flexor digitorum longus (FDL) tendon.
Forefoot:
“Turf Toe” refers to a capsuloligamentous injury of the metatarsophalangeal (MTP) joint of the first toe. The mechanism of injury includes anterior thrust of the metatarsal head in a hyperextended joint with a relatively fixed great toe. This is common in sports played on synthetic turf . . . football, soccer and baseball. There is stretching and tearing of the plantar capsule and tearing of the plantar plate. The plantar plate is a fibrocartilaginous structure that extends from the metatarsal neck to the base of the proximal phalanx. It reinforces the plantar capsule and also attaches the hallux sesamoid bones to the base of the proximal phalanx.
Other common forefoot pathologies in which MRI can be critical include skimboarder’s toe (tear of dorsal capsul), symptomatic hallux valgus (bunion), seasmoid fx/avn, morton’s neuroma, lesser mtp plantar plate tear, and the occasional OCD.
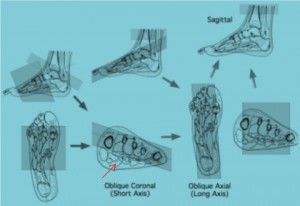
Foot Imaging Planes:
Angle parallel to the 2nd and 3r metatarsal heads on your oblique Coronal
ANKLE/HINDFOOT POSITIONING AND ANATOMY:
The most frequently diseased tendons in the ankle are the Achilles, posterior tibial, and peroneal. MRI can be used to diagnose most disorders of these tendons, as well as stage these disorders to allow appropriate therapy.
Achilles imaging must cover to gastrocnemius insertion
Designated imaging planes Ankle for PTT and Peroneal Pathology
CONCLUSION:
MRI is the gold standard for foot/ankle traumatic injuries and diagnosis of chronic pain/instability syndromes. The high cost of healthcare often puts the patient in the difficult position of determining if a diagnostic test makes economic sense. To help ensure that the referring physician and their patients get true value from the MRI, consult with the ordering Physician and Musculoskeletal Radiologist prior to exam. The right imaging techniques, outstanding image quality and a clinically specific report will ensure optimal diagnosis and treatment for patients.
All-American Teleradiology provides rapid, accurate decisive musculoskeletal MRI interpretations performed by highly experienced, fellowship trained Musculoskeletal Radiologists. Our value added consultative MRI services, to include our providing free MRI accreditation assistance and a Medical Director can help ensure appropriate reimbursement and the highest level of clinical performance.
For more information, email Krysty@allamericanrad.com, call 888-365-5514 or visit www.allamericanrad.com.
Krysty Radabaugh has over 20 years of MRI experience in hospital and outpatient settings. She has served as MRI Coordinator for Cleveland Clinic hospitals; Technical Director for Franklin & Seidelmann Teleradiology; and MRI Accreditation Specialist with national MRI center chain. She has managed MRI centers utilizing a wide range of MRI equipment, which includes: Hitachi, Phillips, GE, Siemens, Toshiba and Esaote. Ms. Radabaugh has worked as a MRI Applications Specialist with Hitachi and Consultant to GE Medical and Bayer Healthcare.